Abstract
Background
The DuoStim protocol has been proposed as an alternative to conventional single and double stimulation cycles in the treatment of infertility. However, its efficacy in improving pregnancy outcomes remains uncertain.
Objective
To systematically evaluate the impact of the DuoStim protocol on pregnancy outcomes in infertile patients by comparing it with single and double conventional stimulation cycles.
Methods
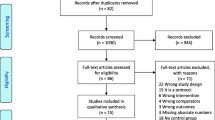
An online systematic search was conducted using PubMed, Cochrane Library, and EMBASE databases, covering the period from their inception to March 2024. Randomized controlled trials (RCTs) comparing the DuoStim protocol with single and double conventional stimulation cycles in infertile patients were identified. Data were extracted by two independent investigators who screened the literature and assessed the quality of the studies. Meta-analysis was performed using RevMan 5.4 software.
Results
A total of six RCTs involving 414 infertile patients were included. The DuoStim protocol significantly increased the total number of oocytes compared to single and double conventional stimulation (MD = − 1.47; 95% CI, − 2.12 to − 0.82; P < 0.00001). There were no statistically significant differences in the number of MII oocytes, total embryos, pregnancy rate, and live birth rate. Subgroup Analysis: compared to single stimulation, the DuoStim protocol significantly increased the number of MII oocytes (MD = 1.71; 95% CI, 0.77 to 2.66; P = 0.0004) and total embryos (MD = 1.34; 95% CI, 0.61 to 2.08; P = 0.0003). There were no significant differences in pregnancy rate and live birth rate. Secondary outcomes showed the effect of the DuoStim protocol in patients undergoing preimplantation genetic testing for aneuploidies (PGT-A). The time to obtain euploid blastocysts was significantly reduced in the DuoStim group compared to the control group (23.3 ± 2.8 days vs. 44.1 ± 2.0 days; P < 0.001).
Conclusions
The DuoStim protocol shows a significant advantage in increasing the total number of oocytes, MII oocytes, and embryos compared to single stimulation. However, it does not significantly improve pregnancy and live birth rates. The protocol also shortens the time to obtain euploid blastocysts in patients undergoing PGT-A, indicating potential benefits for specific patient groups. Further research is needed to confirm these findings and evaluate long-term outcomes. Thus, the quality of evidence should be considered moderate, warranting cautious interpretation of the results.







Similar content being viewed by others
Data Availability
Our study has included all relevant data within the manuscript and supporting materials. If additional data is required for further verification, it is available from the corresponding author upon reasonable request.
References
Sang Q, Ray PF, Wang L. Understanding the genetics of human infertility. Science. 2023;380:158–63.
Zhu Q, Li Y, Ma J, Ma H, Liang X. Potential factors result in diminished ovarian reserve: a comprehensive review. J Ovarian Res. 2023;16:208.
Neves AR, Montoya-Botero P, Sachs-Guedj N, Polyzos NP. Association between the number of oocytes and cumulative live birth rate: a systematic review. Best Pract Res Clin Obstet Gynaecol. 2023;87:102307.
Telfer EE, Grosbois J, Odey YL, Rosario R, Anderson RA. Making a good egg: human oocyte health, aging, and in vitro development. Physiol Rev. 2023;103:2623–77.
Esteves SC, Humaidan P, Roque M, Agarwal A. Female infertility and assisted reproductive technology. Panminerva Med. 2019;61:1–2.
Labarta E. DuoStim: a new strategy proposed for women with poor ovarian response. Fertil Steril. 2020;113:76–7.
Vaiarelli A, Cimadomo D, Argento C, Ubaldi N, Trabucco E, Drakopoulos P, et al. Double stimulation in the same ovarian cycle (DuoStim) is an intriguing strategy to improve oocyte yield and the number of competent embryos in a short timeframe. Minerva Ginecol. 2019;71:372–6.
Sokteang S, Ou P, Tran C, de Ziegler D. Programing the onset of ovarian stimulation: from early follicular phase start to oral contraceptive (OC) pill, to luteal phase E2, Duo-Stim and random start OS protocols. Fertil Steril. 2024;S0015–0282(24):02224–6.
Luo Y, Sun L, Dong M, Zhang X, Huang L, Zhu X, et al. The best execution of the DuoStim strategy (double stimulation in the follicular and luteal phase of the same ovarian cycle) in patients who are poor ovarian responders. Reprod Biol Endocrinol. 2020;18:102.
Sfakianoudis K, Pantos K, Grigoriadis S, Rapani A, Maziotis E, Tsioulou P, et al. What is the true place of a double stimulation and double oocyte retrieval in the same cycle for patients diagnosed with poor ovarian reserve? A systematic review including a meta-analytical approach. J Assist Reprod Genet. 2020;37:181–204.
Glujovsky D, Pesce R, Miguens M, Sueldo CE, Lattes K, Ciapponi A. How effective are the non-conventional ovarian stimulation protocols in ART? A systematic review and meta-analysis. J Assist Reprod Genet. 2020;37:2913–28.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:ED000142.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Boudry L, Mateizel I, Wouters K, Papaleo E, Mackens S, De Vos M, et al. Does dual oocyte retrieval with continuous FSH administration increase the number of mature oocytes in low responders? An open-label randomized controlled trial. Hum Reprod. 2024;39:538–47.
Cerrillo M, Cecchino GN, Toribio M, García-Rubio MJ, García-Velasco JA. A randomized, non-inferiority trial on the DuoStim strategy in PGT-A cycles. Reprod Biomed Online. 2023;46:536–42.
Ghahghayi F, Payandeh A, Najafian A, Ghasemi M, Jabari AJ. Investigating ovulation induction outcomes in patients with decreased ovarian reserve treated with double stimulation during the follicular and luteal phases compared to the conventional antagonist cycle: a randomized clinical trial. Int J Fertil Steril. 2024;18:140–5.
Massin N, Abdennebi I, Porcu-Buisson G, Chevalier N, Descat E, Piétin-Vialle C, et al. The BISTIM study: a randomized controlled trial comparing dual ovarian stimulation (duostim) with two conventional ovarian stimulations in poor ovarian responders undergoing IVF. Hum Reprod. 2023;38:927–37.
Racca A, Rodriguez I, Garcia S, Arroyo G, Polyzos NP. Double versus single stimulation in young low prognosis patients followed by a fresh embryo transfer: a randomized controlled trial (DUOSTIM-fresh). Hum Reprod. 2024;deae104.
Saharkhiz N, Salehpoor S, Hosseini S, Nazari L, Sheibani S, Doohandeh T. Comparison in vitro fertilization outcomes between DouStim and minimal stimulation protocols in poor ovarian responders: a randomized clinical trial. Int J Fertil Steril. 2024;18:135–9.
Vaiarelli A, Cimadomo D, Alviggi E, Sansone A, Trabucco E, Dusi L, et al. The euploid blastocysts obtained after luteal phase stimulation show the same clinical, obstetric and perinatal outcomes as follicular phase stimulation-derived ones: a multicenter study. Hum Reprod. 2020;35:2598–608.
Majumdar A, Majumdar G, Tiwari N, Singh A, Gupta SM, Satwik R. Luteal phase stimulation in the same cycle is an effective strategy to rescue POSEIDON poor responders with no embryos after the first follicular stimulation. J Hum Reprod Sci. 2023;16:218–26.
Puthur SJ, Tracey S, Gould D, Fitzgerald CT. DuoStim protocol- a novel fertility preservation strategy for female oncology patients. Hum Fertil (Camb). 2023;26:1361–7.
Tsampras N, Gould D, Fitzgerald CT. Double ovarian stimulation (DuoStim) protocol for fertility preservation in female oncology patients. Hum Fertil (Camb). 2017;20:248–53.
Rubio C, Simón C, Vidal F, Rodrigo L, Pehlivan T, Remohí J, et al. Chromosomal abnormalities and embryo development in recurrent miscarriage couples. Hum Reprod. 2003;18:182–8.
Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Electronic address: ASRM@asrm.org, Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109:429–36.
Vaiarelli A, Cimadomo D, Gennarelli G, Guido M, Alviggi C, Conforti A, et al. Second stimulation in the same ovarian cycle: an option to fully-personalize the treatment in poor prognosis patients undergoing PGT-A. J Assist Reprod Genet. 2022;39:663–73.
DuoStim - a reproducible strategy to obtain more oocytes and competent embryos in a short time-frame aimed at fertility preservation and IVF purposes. A systematic review - PubMed [Internet]. [cited 2024 Sep 28]. Available from: https://pubmed.ncbi.nlm.nih.gov/32338123/
Fuentes A, García-Ajofrín C, Romero R, Castillo JC, Ortíz JA, Hortal M, et al. Influence of the starting day of luteal phase stimulation on double stimulation cycles. Front Endocrinol (Lausanne). 2023;14:1216671.
Kale A, Kale A. Oocyte Quality and blastocyst formation rate with dual stimulation in patients belonging to POSEIDON Groups 3 and 4: a retrospective comparative study. J Obstet Gynaecol India. 2023;73:57–61.
Saito S, Yamada M, Yano R, Takahashi K, Ebara A, Sakanaka H, et al. Fertility preservation after gonadotoxic treatments for cancer and autoimmune diseases. J Ovarian Res. 2023;16:159.
Author information
Authors and Affiliations
Contributions
Y. Z. contributed to conceptualization, methodology, and writing the original draft. W. L and Y. L. was responsible for data curation and formal analysis. B. L. handled investigation and visualization. L. Z. provided resources and supervision. Z. Y. managed software and validation. K. F. oversaw project administration and funding acquisition. D. L. contributed to reviewing and editing the manuscript. S. C. provided supervision and validation. X. L. contributed to conceptualization, supervision, project administration, and is the corresponding author. All authors have significantly contributed to this work and agree to be accountable for its content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zeng, ., Liu, W., Luo, Y. et al. The impact of Duostim protocol on pregnancy outcomes in infertile patients: A meta-analysis comparing single and double conventional stimulation cycles. J Assist Reprod Genet 41, 3455–3466 (2024). https://doi.org/10.1007/s10815-024-03304-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03304-5