Abstract
Congenital anomalies (CAs) are a leading cause of perinatal and child mortality. With the increasing use of assisted reproductive technology (ART), there is a growing need for research on the health outcomes of children conceived through ART. This systematic review was performed to assess the incidence of CAs in ART-conceived children compared to those conceived naturally. This review followed the PRISMA 2020 guidelines and was registered with PROSPERO. A total of 113 studies were included in this meta-analysis, comprising 768,929 children in the ART group and 40,709,337 children in the control group which comprised spontaneously conceived (SC) children. The primary findings indicated that ART-conceived children have a marginally higher risk of CAs compared to the control group. Subgroup analyses showed that children conceived via ICSI, Day 3 transfer, and fresh embryo transfer (ET) had a slightly higher risk of CAs than those conceived via IVF, Day 5 transfer, or frozen embryo transfer (FET). The study highlights a slightly increased incidence of CAs among ART-conceived children over SC children, underscoring the importance of improving ART methods and closely monitoring the health of these children to reduce the risk of CAs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Background
Congenital anomalies (CAs), more commonly called birth defects, are structural or functional anomalies that develop prior to birth. They include congenital heart defects (CHDs), chromosomal defects such as aneuploidies like Down syndrome, and neural tube defects that lead to poor quality of life and mortality in some cases [1]. Together, they are the primary reason for global perinatal mortality (approximately 2.4 lakh newborns) and global child mortality from ages 1 month to 5 years (equal to around 1.7 lakh children a year). A recent online survey conducted among Southeast Asian countries reported the incidence of birth defects to be 50,000 in 4.6 million children [2]. Chromosomal anomalies like Turner, Edwards, Down, DiGeorge, and Patau syndromes account for 15% of these anomalies, leaving most cases unexplained [3]. CHDs, the most common, occur in 0.76% of live births, rising to 1.5% in stillbirths or terminated pregnancies, highlighting the need for further research [3].
The issues associated with fertility encompass serious social, demographic, as well as medical problems. The World Health Organization (WHO) explains infertility as failure to achieve pregnancy after 12 months or more of regular unprotected sexual intercourse. Roughly one in six people are affected globally with infertility issues. Countries like Poland recommend couples who are trying for conception to directly visit fertility clinics if they are above 40 years of age and to begin with diagnosis and treatment for infertility for couples within 35 years, after unsuccessful attempts [4]. A recent survey-based study in India states that the prevalence of infertility is as high as 24.1 per 1000 women after a duration of marriage of 3 years or more [5]. Assisted reproductive technology (ART) has revolutionized reproductive medicine by aiding conception through in vitro handling and fertilization of gametes. Since the birth of the first in vitro fertilization (IVF) baby in 1978, by performing approximately three million cycles per year, greater than ten million children are credited to be born via ART to date [6, 7]. The advent of procedures in ART like IVF, intracytoplasmic sperm injection (ICSI), and cryopreservation of embryos and gametes, has revolutionized the ART industry [8]. As a result of transferring fewer embryos, rates of healthy pregnancies have increased over this period of time and multiple pregnancy rates have declined, leading to improved neonatal outcomes in several countries [9]. These procedures have become essential tools for overcoming reproductive challenges. However, the increasing use of ART has brought up questions regarding the health of ART-conceived offspring, particularly regarding the risk of CAs [10]. Previous studies have reported an increased incidence of neurological, respiratory, developmental disorders, and facial deformities in ART-conceived children [8]. CAs have been linked to existing demographic parental factors like age, BMI, infertility conditions, and genetic/health problems. The association between ART and CAs tends to reduce after adjusting these factors [9,10,11,12]. Not just ART procedures, but additional interventions like ovulation induction, hormone administration, and other methods are also reported to be added to the risk factors but have not been individually proven as the results available are not consistent [12, 13].
The key focus of this review is to infer from the findings of a wide range of studies that have examined the incidence of CAs in ART-born children compared to spontaneously conceived (SC) children. Even with a heterogeneous collection of studies from various parts of the world, the results reported are inconsistent.
Rationale
The rationale behind this review arises from this lack of consistency and unavailability of meta-analysis studies that include the Indian cohorts with worldwide studies. The existing literature is filled with controversial research outcomes where some present increased incidence and others present inconclusive or contradictory results. The root cause of this heterogeneity arises from the difference with respect to study design, sample size, the criteria chosen for defining CAs, and so on [14]. Possible contributors to this increased incidence include a varied range of ART procedures, from fertilization methods, and cryotechniques to embryo culture techniques and time of embryo transfer. Also, several reviews fail to take parental demographics and infertility conditions into consideration which generates the need for a comprehensive review. Our study aims to provide recent evidence and examine the relationship between ART and CAs through systematic review/meta-analysis [14].
Objectives
This systematic review and meta-analysis primarily intend to evaluate the association between CAs and ART. First, we seek to know the incidence of these anomalies in children born through ART as opposed to SC offspring. By conducting a meta-analysis, we aim to provide more concrete and up-to-date evidence from the literature. We also divided the studies before and after 2015 to check if the results vary in recent times as compared to earlier times, due to advancements in ART. Second, we plan to investigate possible connections between patient demographics, such as underlying infertility issues, and congenital defects seen in children conceived with assisted reproductive technology. Finally, we want to evaluate the impact of different types of ART interventions on the probability of congenital abnormalities in progeny. By achieving these goals, the research hopes to provide insightful knowledge on the efficacy and safety of ART, directing clinical procedures and influencing future investigations in this field of reproductive medicine.
Materials and methods
Methodology and registration
This review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 guidelines (Supplementary Information I) [15]. This review was registered in PROSPERO on 20/05/2024 (ID: CRD42024548861). A protocol was not published prior.
Study selection and eligibility criteria
The population, intervention, comparison, outcome (PICO) criteria was chosen for the systematic review. All the English language studies following these criteria were chosen for the analysis: (1) studies which involved children with congenital defects conceived through ART or naturally, (2) studies reporting on children conceived through many techniques involved in ART were assessed individually (IVF, ICSI, type of embryo transfer (fresh ET or frozen ET), and time of transfer (Day 5 or Day 3), (3) studies which compared the prevalence of CAs in children conceived through ART with children conceived naturally, and (4) all cohort studies, case series, retrospective cohort studies, clinical trials, observational studies, comparative studies, and prospective studies which reported the incidence of CAs in children. No timeline was applied to select the publications.
The studies that were excluded were as follows: (1) studies that focused solely on naturally conceived children; (2) studies that did not report CAs but some other outcome; (3) studies that included non-human subjects; (4) reviews, meta-analyses, editorials, letters, case reports, and commentaries; (5) studies which reported less than 100 cases; and (6) studies which reported other ART interventions without the ones opted in inclusion (hormonal therapy, IUI, etc.) [8].
The studies were grouped based on objectives which included (1) reporting the incidence of CAs in the ART group and natural conception group, (2) reporting the comparison in incidence of CAs in children born to infertile and fertile couples undergoing ART, and (3) reporting the comparison in incidence of congenital defects in children born through different types of ART technique.
Information sources and search strategy
Search was conducted using a combination of key terms and database-specific controlled vocabulary for congenital defects and ART. A comprehensive search was performed in PubMed using keywords and MeSH terms combining them with appropriate Boolean operators and field tags and later adapted for Web of Science, Embase, and Scopus (Supplementary Information II). Only English language articles with human subjects published from database inception till 8th May 2024 were searched. A few studies were also searched manually or taken from references of other studies and reviews to include more relevant studies [3]. All the searches were saved in respective databases and all the studies included were recorded in Zotero [16]. The search was conducted by two independent investigators (PB and AG).
Study screening
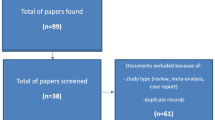
All the screened articles were reviewed by two investigators (PB and AG) using Rayyan, a software platform that facilitates conducting systematic reviews [17]. Discrepancies raised were resolved through discussion or a third reviewer (SU). Studies overlapping in the objectives were added to both data sheets [18, 19] and duplicates were removed with the help of Rayyan software. The whole process was recorded in PRISMA 2020 flowchart for systematic reviews as given in Fig. 1.
Data extraction
The data was collected using a predefined data extraction tool designed on Google Sheets (Supplementary Information III). A set of variables were collected for the analysis which are mentioned below. Various publication details like title, journal, country, year, author, methodological details (types of study, population, and sample characteristics), and the outcome data (numbers and percentages) were extracted. The CAs reported with the history of infertility and type of ART intervention were noted. Any additional interventions which did not fall under the intervention technologies we opted (like the use of donor gametes, preimplantation genetic testing, intrafallopian transfers, and any surgical procedures used) were also noted to remove discrepancies.
Risk of bias assessment
The risk of bias (ROB) was assessed using the case–control studies checklist issued by JBI (The Joanna Briggs Institute) critical appraisal tools [20]. Each study was assessed as per the checklist by two reviewers (PB and AG) independently. The assessment considered the criteria relevant to our systematic review such as study groups, participant identification criteria, statistical analysis, outcome, and other confounding factors (Supplementary Information IV).
Effect measures and data synthesis
The analysis was conducted in Jamovi software, a free and open statistical platform (https://www.jamovi.org/about.html) [21,22,23]. The outcome was assessed in a random effect model (DerSimonian-Laird) using log risk ratios. The risk of bias was also assessed using the Fail-Safe N method (Rosenthal) and outliers were identified with the help of a funnel plot. For one sub-analysis, a fixed effect model was used. The primary outcome was to compare the incidence of CAs in ART-conceived children and SC children. This was obtained using a log risk ratio from 70 studies. The study characteristics were described narratively.
For inclusion, homogeneity in the studies such as standardized outcome measurement, hypothesis, and objectives were taken into consideration. A meta-analysis was conducted for 113 out of 117 articles included by computing the risk ratio in Jamovi. I2test was used to estimate heterogeneity among the selected studies and funnel plot to assess asymmetry (using rank correlation and regression test). Cook’s distance was used to assess outliers in the study groups. A forest plot was created which displayed the risk ratios and confidence intervals.
Results
Study selection
The database search retrieved 1683 articles and after deduplication in Rayyan software, 1415 articles were subjected to title/abstract screening. After removing studies that were irrelevant to the three study objectives, 489 articles were left which were subjected to full-text screening and resulted in 115 articles being included. Additionally, two articles were added from random searches (Fig. 1). From the total 117 studies, 113 were included for analysis since the sample size was not mentioned for the control group for the excluded 4 studies [24,25,26,27]. Seventy studies of 113 were included for the meta-analysis performed for objective 1, and 66 studies of 113 for the meta-analysis done for objective 3.
Characteristics of included studies
To remove potential bias by region, countries from each study were noted. Based on the continental distribution, the maximum studies were obtained from Asia, followed by Europe (Table 1).
Then the studies were assessed for year-wise distribution (Table 2). The maximum number of articles included were post-2010, and a maximum number of papers were obtained from the range 2016–2020.
Nine studies [33, 39, 44, 50, 51, 54, 109, 121, 132] were included for objective 2 where infertility conditions were considered to estimate CAs among infertile and fertile couples who underwent ART. Table 3 describes the percentage of CAs conceived by infertile vs. fertile couples.
ROB or quality assessment
ROB assessment was done using a checklist for case–control studies issued by JBI critical appraisal tools [20]. The studies were subjected to quality assessment by this checklist and 113 studies satisfied the assessment (Supplementary Information IV).
Meta-analysis
Primary outcome: Incidence of congenital defects in ART vs. SC children
A total of 70 studies were included in this meta-analysis to assess the incidence of CAs in ART conceptions as compared to SC using the log risk ratio as the primary outcome measure.
A random-effects model was applied to account for variability across studies, with the DerSimonian-Laird estimator used to calculate the between-study variance (τ2). The pooled estimate of the log risk ratio was μ = 0.327 (95% CI [0.274, 0.381]), indicating a statistically significant positive effect (Z = 12.0, p < 0.001) (Fig. 2a). The log risk ratios observed in individual studies ranged from − 0.618 to 1.494, with 84% of studies reporting a slightly higher incidence of CAs in the ART group compared to the SC group.
a Forest plot analysis comparing incidence of congenital anomalies in ART group (experimental group) vs spontaneous conception group (control group). b Funnel plot depicting the outliers of the meta-analysis which included 70 articles. c Forest plot analysis comparing incidence of congenital anomalies in ART group (experimental group) vs. spontaneous conception group (control group) (pre-2015). d Funnel plot depicting the outliers of the meta-analysis which included 33 articles. e Forest plot analysis comparing incidence of congenital anomalies in ART group (experimental group) vs. spontaneous conception group (control group) (after 2015). f Funnel plot depicting the outliers of the meta-analysis which included 37 articles
Heterogeneity among studies was substantial, as evidenced by Q (69) = 916.815 (p < 0.001), τ2 = 0.032 (SE = 0.0163), and I2 = 92.47%. These statistics indicate that 92.47% of the total variability in effect sizes can be attributed to true heterogeneity rather than sampling error. To further contextualize this variability, a 95% prediction interval was calculated, ranging from − 0.027 to 0.682. This range suggests that while the overall effect is positive, individual studies may yield negative outcomes in specific circumstances. This level of heterogeneity underscores the need to explore potential moderating factors or differences in study design, population characteristics, or intervention implementation.
Outlier and influence diagnostics were conducted to identify studies that may disproportionately affect the results. Two studies [60, 129] were identified as potential outliers, with studentized residuals exceeding the Bonferroni-corrected threshold of ± 3.384. Additionally, Cook’s distances flagged one study [129] as overly influential, indicating that its exclusion might impact the pooled effect size. These findings highlight the importance of considering the influence of specific studies in interpreting the meta-analysis results.
Publication bias was assessed using multiple methods. Neither the rank correlation test (p = 0.578) nor the regression test (p = 0.164) detected funnel plot asymmetry, suggesting minimal evidence of publication bias (Fig. 2b). A fail-safe analysis, conducted using Rosenthal’s approach, revealed a robust fail-safe N = 34,200 (p < 0.001), indicating that 34,200 null-result studies would be required to render the pooled effect size non-significant. This further supports the reliability of the observed effect.
The four studies excluded from the meta-analysis also showed a higher incidence of CAs in ART children compared to SC children [24,25,26,27].
In summary, the meta-analysis demonstrates a statistically significant increase in CAs in the ART group over the SC group. However, the high level of heterogeneity highlights substantial variability in outcomes across studies, suggesting that the effectiveness of ART may depend on contextual or population-specific factors. Outliers and influential studies were identified but did not compromise the robustness of the overall findings. The lack of significant publication bias further strengthens the validity of the results. Future research should explore moderating variables and refine the intervention to optimize its effectiveness across diverse settings.
A comparative analysis of studies done pre- and post-2015 to evaluate the incidence of congenital anomalies in ART children
To find the differences in the incidence of CAs in children born through ART vs. SC, we set the timeline as 2015 to analyze the differences (if any) before and after that year. We sought to find differences caused by advancements in ART and its impact on neonatal health.
Pre-2015
A total of 33 studies published before 2015 were included in this meta-analysis to assess and evaluate the incidence of CAs in children born after ART compared to spontaneously conceived children.
A random-effects model was applied to account for potential variability between studies, with the DerSimonian-Laird estimator used to calculate the between-study variance (τ2 = 0.0149, SE = 0.0074). The estimated log risk ratio was μ = 0.2985 (95% CI: 0.2378 to 0.3593), indicating a statistically significant positive effect (z = 9.6375, p < 0.0001), suggesting that the ART group had slightly higher chances of anomalies than the SC group (Fig. 2c). Observed log risk ratios in individual studies ranged from − 0.6183 to 1.4945, with 85% of studies reporting positive effects.
Heterogeneity analysis revealed a moderate level of variability across studies, with (Q (32) = 104.8409, τ2 = 0.0149, p < 0.0001, and I2 = 69.4776%, suggesting that approximately more than two-thirds of the observed variation in effect sizes is due to differences in true effects rather than random error. This level of heterogeneity suggests that study-level characteristics, such as population demographics, clinical protocols, or contextual differences, may influence the outcomes and require further exploration.
Outlier and influence diagnostics were conducted to identify studies that could disproportionately affect the pooled results. No studies were flagged as outliers based on studentized residuals, as none exceeded the Bonferroni-corrected threshold of ± 3.144. However, Cook’s distances identified one study [45] as overly influential, suggesting that its exclusion might alter the pooled effect size. These findings emphasize the need to carefully interpret the influence of specific studies and consider sensitivity analyses to confirm the robustness of the results.
Publication bias was assessed using both rank correlation and regression tests for funnel plot asymmetry. The rank correlation test did not show significant evidence of asymmetry (p = 0.6781), but the regression test indicated significant funnel plot asymmetry (p = 0.5261), suggesting possible publication bias (Fig. 2d). A fail-safe N analysis, calculated using Rosenthal’s approach, reported a fail-safe N = 3410 (p < 0.001), indicating that 3410 unpublished null-result studies would be needed to nullify the observed pooled effect size. While the fail-safe N indicates robustness, the evidence of funnel plot asymmetry highlights potential biases in the literature, such as selective reporting of positive outcomes.
Post-2015
A total of 37 studies published after 2015 were included in this meta-analysis to assess and evaluate the incidence of CAs in children born after ART compared to spontaneously conceived children.
A random-effects model was applied to account for potential variability between studies, with the DerSimonian-Laird estimator used to calculate the between-study variance (τ2 = 0.0374, SE = 0.0237). The estimated log risk ratio was μ = 0.3532 (95% CI: 0.2766 to 0.4299), indicating a statistically significant positive effect (z = 9.0326, p < 0.0001), suggesting that ART had slightly higher chances of anomalies than SC (Fig. 2e). Observed log risk ratios in individual studies ranged from − 0.445 to 1.296, with 95% of studies reporting positive effects.
Heterogeneity analysis revealed a moderate level of variability across studies, with Q (36) = 794.6589, τ2 = 0.0374, p < 0.0001, and I2 = 95.4698%, suggesting that observed variation in effect sizes is due to differences in true effects. This level of heterogeneity suggests that study-level characteristics, such as population demographics, clinical protocols, or contextual differences, may influence the outcomes and merit further exploration.
Outlier and influence diagnostics were conducted to identify studies that could disproportionately affect the pooled results. Two studies were flagged as outliers based on studentized residuals, as they exceeded the Bonferroni-corrected threshold of ± 3.205 [60, 129]. However, Cook’s distances identified one study as overly influential, suggesting that its exclusion might alter the pooled effect size [129]. These findings emphasize the need to carefully interpret the influence of specific studies and consider sensitivity analyses to confirm the robustness of the results.
Publication bias was assessed using both rank correlation and regression tests for funnel plot asymmetry (Fig. 2f). Neither of these tests showed significant evidence of asymmetry (p = 0.825 and p = 0.227, respectively). A fail-safe N analysis, calculated using Rosenthal’s approach, reported a fail-safe N = 15,953 (p < 0.001), indicating that 15,953 unpublished null-result studies would be needed to nullify the observed pooled effect size. While the fail-safe N indicates robustness, the possibility of selective reporting of positive results cannot be ruled out entirely.
To conclude, this sub-analysis revealed that there were no significant changes observed in the outcome with respect to the timeline employed. The results were consistent and showed slightly higher anomalies in children born via ART vs. SC. Future research should explore the factors contributing to heterogeneity, including study design differences and population-specific characteristics, to better understand the reason. These considerations will help refine the intervention and enhance its generalizability across diverse clinical settings.
Secondary outcomes
Incidence of congenital anomalies in children born after IVF vs. ICSI
A meta-analysis was conducted to evaluate the incidence of CAs conceived through different ART methods, IVF and ICSI. A total of 29 studies were included in this analysis. The fixed effects model yielded a log risk ratio of 0.0877 (95% CI: 0.058 to 0.118, Z = 5.72, p < 0.001), indicating a statistically significant positive association, as shown in the figure below (Fig. 3a). This suggests that ICSI had more effect on outcome than IVF. The 95% confidence interval for the log risk ratio ranged from − 0.277 to 1.440, with 76% of studies reporting positive estimates. These results indicated a statistically significant lower risk of congenital abnormalities for IVF to ICSI, with the negative log risk ratio signifying the reduced risk associated with the IVF group.
The heterogeneity was modest, with I2 = 35.31%, Q (28) = 43.285, p = 0.033, suggesting that approximately one-third of the variability in effect sizes across studies was due to true differences rather than sampling error. Cook’s distances identified three studies [81, 132, 138] as overly influential due to their relatively large weights compared to the rest of the studies. However, evaluation of the studentized residuals showed there was no study which exceeded the value ± 3.1340 and therefore there was no proof of any outliers in the context of this model. Publication bias was assessed using funnel plot asymmetry tests, including the rank correlation and regression tests, neither of which provided evidence of asymmetry (rank correlation: p = 0.211; regression: p = 0.095) (Fig. 3b). The fail-safe N analysis calculated a value of 283 (p < 0.001), indicating that 283 null result studies would be required to nullify this effect indicating the robustness of this analysis.
Overall, this meta-analysis revealed a modest but significant pooled effect size favouring IVF over ICSI with minimal evidence of publication bias and no extreme outliers identified. However, the presence of heterogeneity and influential studies warrants further investigation into study-level characteristics that may explain the observed variability.
Children with congenital anomalies born after fresh ET vs. FET
A total of 30 studies were included in this meta-analysis to assess the efficacy of fresh embryo transfer (ET) compared to frozen embryo transfer (FET) using the log risk ratio as the primary outcome measure. A random-effects model was applied to account for potential variability between studies, with the DerSimonian-Laird estimator used to calculate the between-study variance (τ2 = 0.0199, SE = 0.0121). The pooled estimate of the log risk ratio was μ = 0.117 (95% CI [0.036, 0.199]), indicating a statistically significant positive effect (Z = 2.84, p = 0.005), suggesting that fresh ET has a slightly increased effect on congenital anomalies than FET (Fig. 4a). Observed log risk ratios in individual studies ranged from − 0.465 to 1.565, with 77% of studies reporting positive effects. Despite the overall positive outcome, the prediction interval (− 0.171 to 0.406) reveals that some studies may yield negative results under specific circumstances, highlighting potential variability in intervention effectiveness.
Heterogeneity analysis revealed a moderate level of variability across studies, with Q (29) = 80.772, p < 0.001, and I2 = 64.1%, suggesting that approximately two-thirds of the observed variation in effect sizes is due to differences in true effects rather than random error. The H2 statistic (2.785) further supports this finding, indicating that the total variability in observed effects exceeds the expected variability from sampling error. This level of heterogeneity suggests that study-level characteristics, such as population demographics, clinical protocols, or contextual differences, may influence the outcomes and require further exploration.
Outlier and influence diagnostics were conducted to identify studies that could disproportionately affect the pooled results. No studies were flagged as outliers based on studentized residuals, as none exceeded the Bonferroni-corrected threshold of ± 3.144. However, Cook’s distances identified one study [57] as overly influential, suggesting that its exclusion might alter the pooled effect size. These findings emphasize the need to carefully interpret the influence of specific studies and consider sensitivity analyses to confirm the robustness of the results.
Publication bias was assessed using both rank correlation and regression tests for funnel plot asymmetry. The rank correlation test did not show significant evidence of asymmetry (p = 0.058), but the regression test indicated significant funnel plot asymmetry (p < 0.001), suggesting possible publication bias (Fig. 4b). A fail-safe N analysis, calculated using Rosenthal’s approach, reported a fail-safe N = 247 (p < 0.001), indicating that 247 unpublished null-result studies would be needed to nullify the observed pooled effect size. While the fail-safe N indicates robustness, the evidence of funnel plot asymmetry highlights potential biases in the literature, such as selective reporting of positive outcomes.
In conclusion, this meta-analysis demonstrates a statistically significant pooled effect indicating that fresh ET has an increased effect on anomalies in comparison to FET, with a moderate level of heterogeneity (I2 = 64.1%) indicating variability in study outcomes. Although no extreme outliers were detected, the identification of an influential study and evidence of potential publication bias suggest that the findings should be interpreted cautiously. Future research should explore the factors contributing to heterogeneity, including study design differences and population-specific characteristics, to better understand the contexts in which ET is most effective. These considerations will help refine the intervention and enhance its generalizability across diverse clinical settings.
Children with congenital anomalies born after blastocyst transfer vs. cleavage transfer
A meta-analysis was conducted to evaluate the efficacy of blastocyst-stage embryo transfer (Day 5) compared to cleavage-stage embryo transfer (Day 3) in ART. Seven studies were included, with log risk ratios ranging from − 0.784 to 1.946, and a majority (71%) reporting negative estimates. A random-effects model was applied, using the DerSimonian-Laird estimator to account for between-study variance (τ2 = 0.0952, SE = 0.0805). The pooled log risk ratio was μ = − 0.304 (95% CI [− 0.564, − 0.044], Z = − 2.29, p = 0.022), indicating a statistically significant negative effect favoring blastocyst-stage transfer (Fig. 5a). This suggests that, on average, blastocyst transfer is associated with a lesser incidence of anomalies compared to cleavage-stage transfer. However, the prediction interval (− 0.962 to 0.354) highlights that individual studies may show a positive effect under specific conditions.
Heterogeneity across studies was substantial, with Q (6) = 88.411, p < 0.001, I2 = 93.21%, and H2 = 14.735, suggesting that 93.21% of the observed variability was due to true differences across studies rather than random error. This high degree of heterogeneity underscores the need to examine potential moderating factors, such as population characteristics, study design, or clinical protocols. Outlier analysis, based on studentized residuals, revealed no studies exceeding the Bonferroni-corrected threshold of ± 2.690, and Cook’s distances identified no studies as overly influential. These findings suggest that the results were robust to the influence of individual studies.
Publication bias was assessed through funnel plot asymmetry tests, including the rank correlation and regression tests (Fig. 5b). Neither the rank correlation test (p = 0.773) nor the regression test (p = 0.082) indicated significant asymmetry. Additionally, a fail-safe N = 320 (p < 0.001) was calculated using Rosenthal’s approach, indicating that 320 null-result studies would be required to render the observed effect non-significant. This supports the reliability of the results despite the limited number of included studies.
In conclusion, the meta-analysis demonstrates a statistically significant pooled negative effect, which suggested a slightly reduced risk with blastocyst-stage embryo transfer. However, the substantial heterogeneity across studies (I2 = 93.21%) and the prediction interval suggest that the results may not be consistent across all contexts. No evidence of publication bias was detected, and the findings appeared robust to the influence of individual studies. Further research is warranted to explore the factors contributing to variability in outcomes and to better understand the conditions under which blastocyst transfer might achieve optimal efficacy. These results have important implications for clinical decision-making in assisted reproductive technology, highlighting the need for tailored approaches to embryo transfer based on patient-specific and contextual factors.
The meta-analyses showed a different profile for the risk of congenital abnormalities connected to distinct ART methods. Reduced risk was noted when IVF was used instead of ICSI, FET was used instead of fresh ET, and blastocyst-stage transfer was used instead of cleavage-stage transfer. These results are useful for understanding the risks and benefits of various ART interventions to make better informed clinical decisions in ART applications and to improve future studies of reproductive healthcare.
Discussion
General interpretations
The result of the current systematic review and meta-analysis revealed a statistically significant increase in the incidence of CAs in children born after ART compared with children born after SC Our study included 117 studies (3 of them from the Indian cohort) in which 70 studies were chosen for meta-analysis for comparison of anomalies in ART vs. SC group. This included 768,929 children in the ART group and 40,709,337 children in the SC group. This provided a comprehensive robust result. This analysis revealed an average log risk ratio of 0.328, translating to an approximately 39% increase in the risk of CAs for ART-conceived children. This aligns with previous meta-analyses [14, 139, 140] which had a similar result as ours. While this increase in relative risk sounds substantial, the absolute risk difference must be placed in context. The incidence of CAs was set around 2.48% for SC children in the included studies; thus, the estimated incidence for ART-conceived children, when applying this 39% relative increase observed in our analysis, is 3.45%, resulting in an absolute risk difference of 0.97 percentage points (approximately 1%).
Thus, while there is a slight elevation in risk with ART, the absolute increase is clinically modest. Such information should be communicated to physicians and potential parents effectively so that they underscore the importance of deeper understanding and informed decision making when it comes to ART. A recent meta-analysis on the same topic also suggested the same but just for major anomalies [141]. Our study covered a more comprehensive analysis due to the higher number of studies included and more subgroup analysis (ET vs. FET, day 5 vs. day 3 transfer) which shed insights on the types of ART treatment and their potential effect.
Our analysis identified variability in risk depending on the specific ART technique used. For instance, children conceived through IVF showed a lower risk of CAs compared to those conceived via ICSI, while Day 5 transfer and FET showed lower risk compared to that of day 3 transfer and fresh ET.
Limitations
There are some strengths and limitations associated with the reviewed source regarding the identification of the evidence. The strengths could be ascribed to the permissiveness of the papers encompassing large heterogeneity revealed by high I2 values declared in meta-analysis. However, the increased risk of CAs are not solely from ART but they could also originate from pre-existing and uncontrollable factors such as maternal age, lifestyle factors, fertility issues, genetics, and other health conditions. Studies like these help in deeper understanding of the origin of these anomalies and the role ART might have in it.
-
Advanced maternal age: One of the more significant confounders for CAs may include advanced maternal age [98, 114]. As maternal age increases, chromosomal abnormalities and other anomalies rise. This is often confounded by selection for ART patients, as many ART patients tend to be older and might therefore be suffering from infertility.
-
Infertility and subfertility: Couples initiating ART may have a pre-diagnosed fertility disorder in either or both male and female partners linked with several associated medical conditions, and these preconditions have contributed to increasing CA disposition risk. Infertility can arise in women with, among countless other possible causes, advanced maternal age, polycystic ovary syndrome (PCOS), or endometriosis.
-
Health conditions: Many ART patients may have pre-existing health conditions such as diabetes, hypertension, thyroid disorders, or obesity. These are known to increase the risk of adverse pregnancy outcomes. For example, maternal diabetes is associated with a higher risk of neural tube defects and other CAs [142]. Conditions like these may confound the relationship between ART and congenital anomalies.
-
Lifestyle factors: Factors such as smoking, alcohol consumption, diet, and physical activity may also be implicated in the risk of CAs. While these factors are important to consider within any population, they may, nevertheless, be more prevalent or exert different effects on ART treatments.
-
Genetic predispositions and family history: The genetic factors have a significant role in affecting the offspring’s health which may get transmitted independently of ART intervention. In addition, some ART treatments involve genetic screening and preimplantation genetic testing, which could reveal genetic abnormalities that might be missed otherwise in natural pregnancies. Such variations have the net effect of making accounting for these variables less routine, which influences the overall quality of the risk estimates that are tied to ART.
Moreover, mainly because of the type of studies in the sample, the existence of outliers within the sample or influential studies poses a great deal of confusion in the results displayed. First, given the logistic nature of the models utilized, the relationship between the covariates and time-to-event outcomes may be non-linear and non-proportional, which could be factors for confounding in case of imbalance in the covariate distribution between the treatment groups, though balanced randomization was employed in the present study [143, 144].
It should also be pointed out that only studies reported in the English language have been included in the current analysis. Such a language limitation might exclude some relevant data from such research works that are in languages other than English. Therefore, it introduces a limitation of language bias, and this reaffirms the fact that the results cannot be generalized.
Another limitation connected with the systematic review is the potential of reporting bias because only studies that have been published have been included. No publication bias of the primary outcome is identified when considering the funnel plot; nevertheless, it can be envisaged that many similar studies were not published at all and, therefore, affected the outlook of the results.
Implications of the results and future directions
Therefore, the findings of this review are helpful to clinicians, policymakers, and researchers who are concerned about prospective parents and fulfilling their natural desire for offspring and improving their patients’ quality of life. In understanding the study conducted above, clinicians and reproductive specialists should note that birth through ART exposes a newborn to anomalies more than natural conception. It is necessary to present such information specifically for the decision-making referring to the choice of ART procedures. It is to be emphasized that each couple should think about the possible risks and benefits of their future reproductive decisions in order to make a conscious and well-informed decision.
In the practice of ART, timing of embryo transfer is critical to the success and safety of the treatment. As to the comparative risks of embryo transfer on day 3 as opposed to day 5, very little research has been done. The present review emphasizes the need for further studies to see how timing of transfer may influence the subsequent incidence of CAs. Since embryos at different stages may possess different implantation and developmental capabilities, these variations could affect their long-term outcomes. Future studies should be conducted to compare these transfer strategies while controlling for confounding factors to see if the specific timing of transfer leads to a lower risk of CAs in the long term.
Another important finding of this review is the marginally increased risk of CAs in children conceived with fresh ETs compared to those conceived through FETs [64, 128]. While there have been quite favorable outcomes from FETs, fresh ETs are still being conducted. The reasons for this increased risk are unclear, but they may include the hormonal environment during the cycle in which fresh ET takes place, embryo stage at the time of transfer, or maternal–fetal interactions [145]. Thus, it will be of great importance for future studies to investigate the physiological differences between these two transfer methods, as knowledge of these factors could allow for optimization of ART procedures in an attempt to reduce risks.
Apart from timing and technique of embryo transfer, other ART-related factors such as hormonal treatment for uterine preparation or use of PGD should also be given due consideration. Hormonal treatment, in particular, can have long-lasting effects on embryonic and fetal development. Moreover, socio-economic and lifestyle factors must be considered, along with maternal health, to enable such research to be conducted.
To address the limitations of our study, studies should focus on more confounding factors to find the root cause of CAs. Along with this, establishing a longitudinal follow-up of ART-conceived children is crucial in establishing the entire spectrum of health risks associated with ART treatment, including CAs, developmental disorders, and long-term health effects. Larger scale and methodologically better-designed cohort studies should be done involving children born through ART compared with those born without ART usage and compared while statistically controlling for such potential confounders as parents’ age, size, and socio-economic status. In addition, future studies should also focus on providing detailed information on the effect of various other ART interventions such as hormonal treatments, preimplantation genetic testing, culture conditions and other practices on the incidence of CAs in ART-conceived children to bring refinements in ART.
Conclusion
To summarize, this systematic review and meta-analysis aimed to offer a detailed understanding of the study objective which was to examine the odds of CAs in ART children as compared to children conceived naturally. The preliminary results of this research show that ART-conceived offspring have a slightly higher rate of birth defects.
The secondary analysis builds upon this discussion by reemphasizing the fact that implementing different ART methods entails disparate risks for children and families. Most of the studies with matched samples were therefore informative; it was noted that the meta-analysis of the current comparative studies of IVF and ICSI indicated a statistically significant lower risk of CAs associated with IVF than with ICSI. Fresh ET had a slightly higher incidence of anomalies in children as compared to FET. The analysis also revealed that cleavage-stage transfer posed a slightly higher risk of CAs as compared to blastocyst transfer. Furthermore, amid other perceived factors, the analysis of the study and use of underlying causes of infertility among parents establish that CA risk also depends on parental factors. This calls for the need to consider the parents’ characteristics as well as the specific infertility factors when evaluating the possibility of the increased risk for CAs. The results are summarized and tabulated in Table 4.
Therefore, as affirmed by this systematic review and meta-analysis, there is importance in carrying out regular follow-up of the health of children conceived through ART. The finding of this study should help enlighten clinical practices, by offering directions on how the ART should be practiced, together with the counseling that should accompany it in prospective parentage. Although the available options for the treatment of infertility continue to evolve, it is crucial to align the positive impact of ART with the identification of adverse outcomes for the sake of future generations.
Data availability
Not applicable as no new data were created in the study as it is a systematic review and meta-analysis. All data analyses are included in the manuscript and supplementary information. This review was registered in PROSPERO on 20/05/2024 (ID: CRD42024548861), as mentioned in the “Materials and methods” section.
References
Congenital disorders [Internet]. [cited 2024 Apr 8]. Available from: https://www.who.int/news-room/fact-sheets/detail/birth-defects
World Birth Defects Day: every journey matters [Internet]. [cited 2024 Jul 4]. Available from: https://www.who.int/southeastasia/news/detail/02-03-2024-world-birth-defects-day-every-journey-matters.
Giorgione V, Parazzini F, Fesslova V, Cipriani S, Candiani M, Inversetti A, et al. Congenital heart defects in IVF/ICSI pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(1):33–42.
Serafin D, Grabarek BO, Boroń D, Madej A, Cnota W, Czuba B. Evaluation of the risk of birth defects related to the use of assisted reproductive technology: an updated systematic review. Int J Environ Res Public Health. 2022;19(8):4914.
Agiwal V, Madhuri RS, Chaudhuri S. Infertility burden across indian states: insights from a nationally representative survey conducted during 2019–21. J Reprod Infertil. 2023;24(4):287–92.
Steel AJ, Sutcliffe A. Long-term health implications for children conceived by IVF/ICSI. Hum Fertil. 2009;12(1):21–7.
Eisenberg E. Long-term outcomes in children born after assisted conception. Semin Reprod Med. 2012;30(2):123–30.
Zhang Z, Liu X, Wei C, Luo J, Shi Y, Lin T, et al. Assisted reproductive technologies and the risk of congenital urogenital tract malformations: a systematic review and meta-analysis. J Pediatr Urol. 2021;17(1):9–20.
Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ. Assisted reproductive technologies and the risk of birth defects–a systematic review. Hum Reprod. 2005;20(2):328–38.
Kurinczuk JJ, Hansen M, Bower C. The risk of birth defects in children born after assisted reproductive technologies. Curr Opin Obstet Gynecol. 2004;16(3):201–9.
Tararbit K, Houyel L, Bonnet D, De Vigan C, Lelong N, Goffinet F, et al. Risk of congenital heart defects associated with assisted reproductive technologies: a population-based evaluation. Eur Heart J. 2011;32(4):500–8.
Lv H, Diao F, Du J, Chen T, Meng Q, Ling X, et al. Assisted reproductive technology and birth defects in a Chinese birth cohort study. Lancet Regional Health-Western Pacific. 2021;7:100090.
Fatima P, Hossain MM, Rahman D, Suman GM. Outcome of pregnancies after inadvertent exposure to GnRH agonist in early pregnancy. Mymensingh Med J. 2011;20(2):303–7.
Qin J, Sheng X, Wang H, Liang D, Tan H, Xia J. Assisted reproductive technology and risk of congenital malformations: a meta-analysis based on cohort studies. Arch Gynecol Obstet. 2015;292(4):777–98.
PROSPERO [Internet]. [cited 2024 Jul 24]. Available from: https://www.crd.york.ac.uk/prospero/about.php?about=citerecord.
Zotero | Your personal research assistant [Internet]. [cited 2024 May 28]. Available from: https://www.zotero.org/
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Raja EA, Bhattacharya S, Maheshwari A, McLernon DJ. A comparison of perinatal outcomes following fresh blastocyst or cleavage stage embryo transfer in singletons and twins and between singleton siblings. Hum Reprod Open [Internet]. 2023;2023(2). Available from: https://www.embase.com/search/results?subaction=viewrecordandid=L2024679212andfrom=exportU2-L2024679212.
Wen S, Miao Q, Taljaard M, Lougheed J, Gaudet L, Davies M, et al. Associations of assisted reproductive technology and twin pregnancy with risk of congenital heart defects. JAMA Pediatr. 2020;174(5):446–54.
JBI Critical Appraisal Tools | JBI [Internet]. 2020. Available from: https://www.jbi.global/critical-appraisal-tools. Accessed 3 Dec 2024.
jamovi - open statistical software for the desktop and cloud [Internet]. [cited 2024 Jul 22]. Available from: https://www.jamovi.org/
Conducting Meta-Analyses in R with the metafor Package | Journal of Statistical Software [Internet]. [cited 2024 Jul 22]. Available from: https://www.jstatsoft.org/article/view/v036i03
The Comprehensive R Archive Network [Internet]. [cited 2024 Jul 22]. Available from: https://cran.r-project.org/
Galdini A, Fesslova VME, Gaeta G, Candiani M, Pozzoni M, Chiarello C, et al. Prevalence of congenital heart defects in pregnancies conceived by assisted reproductive technology: a cohort study. J Clinic Med. 2021;10(22). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85119172992&doi=10.3390%2fjcm10225363&partnerID=40&md5=580227aec7428088f28e3672c1af8d5a
Banker M, Arora P, Banker J, Benani H, Shah S, Lalitkumar PGL. Prevalence of structural birth defects in IVF-ICSI pregnancies resulting from autologous and donor oocytes in Indian sub-continent: results from 2444 births. Acta Obstet Gynecol Scand. 2019;98(6):715–21.
Hourvitz A, Pri-Paz S, Dor J, Seidman DS. Neonatal and obstetric outcome of pregnancies conceived by ICSI or IVF. Reprod BioMed Online. 2005;11(4):469–75.
Pregnancies and births resulting from in vitro fertilization: french national registry, analysis of data 1986 to 1990. FIVNAT (French in vitro National). Fertil Steril. 1995;64(4):746–56.
Farhi A, Reichman B, Boyko V, Mashiach S, Hourvitz A, Margalioth EJ, et al. Congenital malformations in infants conceived following assisted reproductive technology in comparison with spontaneously conceived infants. J Matern Fetal Neonatal Med. 2013;26(12):1171–9.
Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X, Cao Y, et al. Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. New Engl J Med. 2016;375(6):523–33.
Han Y, Luo H, Zhang Y. Congenital anomalies in infants conceived by infertile women through assisted reproductive technology: a cohort study 2004–2014. Exp Ther Med. 2018;16(4):3179–85.
Iwashima S, Ishikawa T, Itoh H. Reproductive technologies and the risk of congenital heart defects. Hum Fertil. 2017;20(1):14–21.
Xiong Y, Zang X, Xie T, Yang C, Jiang X, Chen M. Additional adverse perinatal outcomes with no effect on neonatal mortality and birth defects in pregnancies conceived by assisted reproductive technology. Frontiers in Pediatrics. 2022;10:809259.
Chen L, Li D, Ni X, Zhu L, Zhang N, Fang J, et al. Effects of the normal sperm morphology rate on the clinical and neonatal outcomes of conventional IVF cycles. Andrologia. 2020;52(5):e13568.
Ooki S. Birth defects after assisted reproductive technology according to the method of treatment in Japan: nationwide data between 2004 and 2012. Environmental Health and Preventive Medicine. 2015;20(6):460–5.
Shahverdi E, Roodsari F, Saffar M. Comparison of birth defects in infants conceived by assisted reproductive technologies vs. naturally conceived infants in Mashhad, Iran. GalenMedical Journal. 2015;4(4):146–50.
Chang H, Hwu W, Chen C, Hou C, Cheng W. Children conceived by assisted reproductive technology prone to low birth weight, preterm birth, and birth defects: a cohort review of more than 50,000 live births during 2011–2017 in Taiwan. Frontiers in Pediatrics. 2020;8:87.
Kuwata T, Matsubara S, Ohkuchi A, Watanabe T, Izumi A, Honma Y, et al. The risk of birth defects in dichorionic twins conceived by assisted reproductive technology. Twin Res. 2004;7(3):223–7.
Li F, Duan X, Li M, Ma X (2024) Sperm DNA fragmentation index affect pregnancy outcomes and offspring safety in assisted reproductive technology. Sci Rep 14(1). https://doi.org/10.1038/s41598-023-45091-6.
Aliani F, Haghshenas Z, Dizaj A, Arabipoor A, Vesali S, Ashrafi M. Birth prevalence of genital anomalies among males conceived by intracytoplasmic sperm injection cycles: a cross-sectional study. International Journal of Reproductive Biomedicine. 2023;21(1):53–60.
Zeng J, Yao Z, Zhang Y, Tian F, Liao T, Wu L, et al. Fertilization and neonatal outcomes after early rescue intracytoplasmic sperm injection: a retrospective analysis of 16,769 patients. Archives of Gynecology and Obstetrics. 2022;306(1):249–58.
Xiong F, Sun Q, Li G, Yao Z, Chen P, Wan C, et al. Perinatal and neonatal outcomes of pregnancies after early rescue intracytoplasmic sperm injection in women with primary infertility compared with conventional intracytoplasmic sperm injection: a retrospective 6-year study. BMC Pregnancy and Childbirth. 2020;20(1):460.
Parsafar Z, Dehghani-Firouzabadi R. Comparing the pregnancy outcomes of cleavage and blastocyst stage in frozen embryo transfer cycles: a cross-sectional study. International Journal of Reproductive Biomedicine. 2023;21(11):929–36.
Hershko-Klement A, Sukenik-Halevy R, Biron Shental T, Miller N, Berkovitz A. Intracytoplasmic morphologically selected sperm injection and congenital birth defects: a retrospective cohort study. Andrology. 2016;4(5):887–93.
Hu S, Xu B, Huang B, Jin L. The impact of male infertility or intracytoplasmic sperm injection technique on perinatal outcomes. Journal of Maternal-Fetal and Neonatal Medicine. 2022;35(4):685–91.
Merlob P, Sapir O, Sulkes J, Fisch B. The prevalence of major congenital malformations during two periods of time, 1986–1994 and 1995–2002 in newborns conceived by assisted reproduction technology. Eur J Med Genet. 2005;48(1):5–11.
Liao YJ, Fang NW, Yao CS, Chang JT, Wang HP. Neonatal outcomes in infants conceived using assisted reproductive technologies: a single medical center cohort study. Pediatrics and Neonatology. 2024;65(5):469–75.
Noda A, Ishikuro M, Obara T, Murakami K, Ueno F, Matsuzaki F, et al. Association between maternal infertility treatment and child neurodevelopment: findings from the Tohoku Medical Megabank Project Birth and Three-Generation Cohort Study in Miyagi and Iwate Prefectures, Japan. BMJ Open [Internet]. 2022;12(6). Available from: https://www.embase.com/search/results?subaction=viewrecordandid=L638209163andfrom=export U2 - L638209163.
Yin C, Li LJ, Ma S, Zhao H, Xu L, Li C, et al. Efficiency and safety of laser-assisted hatching on vitrified-warmed blastocyst transfer cycles: a prospective control trial. Lasers Med Sci. 2022;37(3):1931–42.
Liu C, Chen H, Zhao J, Chen Y, Xu B. Comparative study on risk of birth defects in singleton ART birth under high levels of estrogen after fresh embryo transfer and frozen embryo transfer. J Matern-Fetal Neonatal Med. 2022;35(25):9536–43.
Hu S, Xu B, Jin L. Perinatal outcome in young patients with diminished ovarian reserve undergoing assisted reproductive technology. Fertil Steril. 2020;114(1):118-124.e1.
Zhou WJ, Huang C, Jiang SH, Ji XR, Gong F, Fan LQ, et al. Influence of sperm morphology on pregnancy outcome and offspring in in vitro fertilization and intracytoplasmic sperm injection: a matched case-control study. Asian J Androl. 2021;23(4):421–8.
Zhang L, Zhang W, Xu H, Liu K. Birth defects surveillance after assisted reproductive technology in Beijing: a whole of population-based cohort study. BMJ Open [Internet]. 2021;11(6). Available from: https://www.embase.com/search/results?subaction=viewrecordandid=L635357517andfrom=exportU2-L635357517.
Yan J, Guan Y, Fan H, Mu M, Sun S, Geng W, et al. Neonatal outcomes of singleton live births with vanishing twin syndrome following double embryos transfer in assisted reproductive technology: a retrospective cohort study. J Ovarian Res [Internet]. 2019;12(1). Available from: https://www.embase.com/search/results?subaction=viewrecordandid=L628577714andfrom=export.
Jwa S, Jwa J, Kuwahara A, Irahara M, Ishihara O, Saito H. Male subfertility and the risk of major birth defects in children born after in vitro fertilization and intracytoplasmic sperm injection: a retrospective cohort study. BMC Pregnancy and childbirth. 2019;19:19.
Heo JS, Lee HJ, Lee MH, Choi CW. Comparison of neonatal outcomes of very low birth weight infants by mode of conception: in vitro fertilization versus natural pregnancy. Fertil Steril. 2019;111(5):962–70.
Zhu J, Zhu Q, Wang Y, Wang B, Lyu Q, Kuang Y. Comparative study on risk for birth defects among infants after in vitro fertilization and intracytoplasmic sperm injection. Syst Biology Reprod Med. 2019;65(1):54–60.
Zhou Z, Chen L, Wu H, Zheng D, Li R, Mol BW, et al. Assisted reproductive technology in Beijing, 2013–2015. Reprod BioMed Online. 2018;37(5):521–32.
Yang M, Fan XB, Wu JN, Wang JM. Association of assisted reproductive technology and multiple pregnancies with the risks of birth defects and stillbirth: a retrospective cohort study. Sci Rep. 2018;8(1):8296.
Yu H, Yang Q, Sun X, Chen G, Qian N, Cai R, et al. Association of birth defects with the mode of assisted reproductive technology in a Chinese data-linkage cohort. Fertility and sterility. 2018;109(5):849–56.
Qin J, Sheng X, Wu D, Gao S, You Y, Yang T, et al. Adverse obstetric outcomes associated with in vitro fertilization in singleton pregnancies: a prospective cohort study. Reprod Sci. 2017;24(4):595–608.
Jie Z, Yiling D, Ling Y. Association of assisted reproductive technology with adverse pregnancy outcomes. Int J Reprod Biomed. 2015;13(3):169–80.
Yan J, Huang G, Sun Y, Zhao X, Chen S, Zou S, et al. Birth defects after assisted reproductive technologies in China: analysis of 15,405 offspring in seven centers (2004 to 2008). FERTILITY AND STERILITY. 2011;95(1):458–60.
Fujii M, Matsuoka R, Bergel E, Van Der Poel S, Okai T. Perinatal risk in singleton pregnancies after in vitro fertilization. Fertil Steril. 2010;94(6):2113–7.
Li H, Qiao J, Chi H, Chen X, Liu P, Ma C. Comparison of the major malformation rate of children conceived from cryopreserved embryos and fresh embryos. Chin Med J. 2010;123(14):1893–7.
Yin L, Hang F, Gu LJ, Xu B, Ma D, Zhu GJ. Analysis of birth defects among children 3 years after conception through assisted reproductive technology in China. Birth Defects Res A Clin Mol Teratol. 2013;97(11):744–9.
Farhangniya M, Dortaj Rabori E, Mozafari Kermani R, Haghdoost AA, Bahrampour A, Bagheri P, et al. Comparison of congenital abnormalities of infants conceived by assisted reproductive techniques versus infants with natural conception in Tehran. International Journal of Fertility and Sterility. 2013;7(3):217–24.
Poon WB, Lian WB. Perinatal outcomes of intrauterine insemination/clomiphene pregnancies represent an intermediate risk group compared with in vitro fertilisation/ intracytoplasmic sperm injection and naturally conceived pregnancies. J Paediatr Child Health. 2013;49(9):733–40.
Zhang N, Tian T, Li J, Zhu X, Jiesisibieke D, Fang S, et al. A comparison of pregnancy outcomes and congenital malformations in offspring between patients undergoing intracytoplasmic sperm injection and conventional in vitro fertilization: a retrospective cohort study. Fertil Steril. 2024;121(6):982–90.
Rama Raju GA, Jaya Prakash G, Murali Krishna K, Madan K. Neonatal outcome after vitrified day 3 embryo transfers: a preliminary study. Fertil Steril. 2009;92(1):143–8.
Singh N, Malhotra N, Mahey R, Patel G, Saini M. In vitro fertilization as an independent risk factor for perinatal complications: single-center 10 years cohort study. J Bras Reproducao Assistida. 2023;27(2):197–203.
Sánchez Soler MJ, López-González V, Ballesta-Martínez MJ, Gálvez-Pradillo J, Nicolás-Arnao M, Gómez-Sánchez E, et al. Risk of major and minor birth defects in children conceived by assisted reproductive technology (IVF/ICSI): A prospective controlled cohort study. Anales de Pediatria. 2021;95(6):448–58.
Levi Setti PE, Moioli M, Smeraldi A, Cesaratto E, Menduni F, Livio S, et al. Obstetric outcome and incidence of congenital anomalies in 2351 IVF/ICSI babies. J Assist Reprod Genet. 2016;33(6):711–7.
Zhu J, Basso O, Obel C, Bille C, Olsen J. Infertility, infertility treatment, and congenital malformations: Danish national birth cohort. BMJ-BRITISH MEDICAL JOURNAL. 2006;333(7570):679.
Fauque P, De Mouzon J, Devaux A, Epelboin S, Gervoise-Boyer M, Levy R, et al. Do in vitro fertilization, intrauterine insemination or female infertility impact the risk of congenital anomalies in singletons? A longitudinal national French study. Hum Reprod. 2021;36(3):808–16.
Katalinic A, Rösch C, Ludwig M, German ICSI Follow-Up Study Group. Pregnancy course and outcome after intracytoplasmic sperm injection: a controlled, prospective cohort study. Fertil Steril. 2004;81(6):1604–16.
Bonduelle M, Liebaers I, Deketelaere V, Derde MP, Camus M, Devroey P, et al. Neonatal data on a cohort of 2889 infants born after ICSI (1991–1999) and of 2995 infants born after IVF (1983–1999). Hum Reprod. 2002;17(3):671–94.
Klemetti R, Gissler M, Sevón T, Koivurova S, Ritvanen A, Hemminki E. Children born after assisted fertilization have an increased rate of major congenital anomalies. FERTILITY AND STERILITY. 2005;84(5):1300–7.
Couck I, Van Nylen L, Deprest J, Lewi L. Monochorionic twins after in-vitro fertilization: do they have poorer outcomes? Ultrasound Obstet Gynecol. 2020;56(6):831–6.
Marton V, Zadori J, Kereszturi A, Kozinszky Z. Associated perinatal determinants of vanishing twin pregnancies achieved by in vitro fertilization vs. spontaneous conception. Arch Gynecol Obstet. 2020;301(2):491–8.
Ståhl O, Boyd H, Giwercman A, Lindholm M, Jensen A, Kjær S, et al. Risk of birth abnormalities in the offspring of men with a history of cancer: a cohort study using Danish and Swedish national registries. JNCI-J National cancer institute. 2011;103(5):398–406.
Malchau S, Loft A, Larsen E, Henningsen A, Rasmussen S, Andersen A, et al. Perinatal outcomes in 375 children born after oocyte donation: a Danish national cohort study. FERTILITY AND STERILITY. 2013;99(6):1637.
Setti P, Albani E, Morenghi E, Morreale G, Delle Piane L, Scaravelli G, et al. Comparative analysis of fetal and neonatal outcomes of pregnancies from fresh and cryopreserved/thawed oocytes in the same group of patients. FERTILITY AND STERILITY. 2013;100(2):396–401.
Bensdorp A, Hukkelhoven C, van der Veen F, Mol B, Lambalk C, van Wely M. Dizygotic twin pregnancies after medically assisted reproduction and after natural conception: maternal and perinatal outcomes. Fertil Steril. 2016;106(2):371-U190.
Sargisian N, Lannering B, Petzold M, Opdahl S, Gissler M, Pinborg A, et al. Cancer in children born after frozen-thawed embryo transfer: a cohort study. Hum Reprod. 2022;37((Sargisian N.; Bergh C.; Wennerholm U.B.) Institute of Clinical Sciences-Sahlgrenska Academy, University of Gothenburg-Sahlgrenska University Hospital, Department of obstetrics and gynecology, Gothenburg, Sweden):i161.
Di Tommaso M, Sisti G, Colombi I, Seravalli V, Malosso E, Vannuccini S, et al. Influence of assisted reproductive technologies on maternal and neonatal outcomes in early preterm deliveries. J Gynecology Obstetrics and human reproduction. 2019;48(10):845–8.
Aydin CA, Aydin S, Serdaroǧlu H. Multifetal gestations with assisted reproductive technique before the single-embryo transfer legislation: obstetric, neonatal outcomes and congenital anomalies. Journal of Maternal-Fetal and Neonatal Medicine. 2016;29(15):2475–80.
Nouri K, Ott J, Stoegbauer L, Pietrowski D, Frantal S, Walch K. Obstetric and perinatal outcomes in IVF versus ICSI-conceived pregnancies at a tertiary care center—a pilot study. Reproductive Biology and Endocrinology [Internet]. 2013;11(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84883185014anddoi=10.1186%2f1477-7827-11-84andpartnerID=40andmd5=d4b548b2d53edfaa6230f78ee873d4fd.
Ferraz Liz C, Domingues S, Guedes A, Lopes L. The impact of chorionicity and assisted reproductive therapies in obstetric and neonatal outcomes. Journal of Maternal-Fetal and Neonatal Medicine. 2022;35(8):1439–44.
Henningsen AKA, Opdahl S, Wennerholm UB, Tiitinen A, Rasmussen S, Romundstad LB, et al. Risk of congenital malformations in live-born singletons conceived after intracytoplasmic sperm injection: a Nordic study from the CoNARTaS group. Fertil Steril. 2023;120(5):1033–41.
Maheshwari A, Bell JL, Bhide P, Brison D, Child T, Chong HY, et al. Elective freezing of embryos versus fresh embryo transfer in IVF: A multicentre randomized controlled trial in the UK (E-Freeze). Hum Reprod. 2022;37(3):476–87.
Algeri P, Ornaghi S, Vaglio Tessitore I, Brienza L, Cozzolino S, Incerti M, et al. Delivery and feto-neonatal outcomes of diamniotic twin pregnancies in women with no chronic disease or gestational complications: impact of mode of conception. J Matern-Fetal Neonatal Med. 2020;33(12):2081–8.
Spangmose AL, Ginström Ernstad E, Malchau S, Forman J, Tiitinen A, Gissler M, et al. Obstetric and perinatal risks in 4601 singletons and 884 twins conceived after fresh blastocyst transfers: a nordic study from the CoNARTaS group. Hum Reprod. 2020;35(4):805–15.
Pontesilli M, Hof M, Ravelli A, van Altena A, Soufan A, Mol B, et al. Effect of parental and ART treatment characteristics on perinatal outcomes. Hum Reprod. 2021;36(6):1640–65.
Marconi N, Raja EA, Bhattacharya S, Maheshwari A. Perinatal outcomes in singleton live births after fresh blastocyst-stage embryo transfer: a retrospective analysis of 67 147 IVF/ICSI cycles. Hum Reprod. 2019;34(9):1716–25.
Rahu K, Allvee K, Karro H, Rahu M. Singleton pregnancies after in vitro fertilization in Estonia: a register-based study of complications and adverse outcomes in relation to the maternal socio-demographic background. BMC PREGNANCY AND CHILDBIRTH. 2019;19:19.
Henningsen A, Bergh C, Skjaerven R, Tiitinen A, Wennerholm U, Romundstad L, et al. Trends over time in congenital malformations in live-born children conceived after assisted reproductive technology. Acta Obstet Gynecol Scand. 2018;97(7):816–23.
Sunkara SK, Antonisamy B, Selliah HY, Kamath MS. Perinatal outcomes after gestational surrogacy versus autologous IVF: analysis of national data. Reprod BioMed Online. 2017;35(6):708–14.
Beyer DA, Amari F. Maternal risk factors and neonatal outcomes after ART treatment—a German monocenter experience. Middle East Fertil Soc J. 2016;21(3):155–60.
Ginström Ernstad E, Bergh C, Khatibi A, Källén KBM, Westlander G, Nilsson S, et al. Neonatal and maternal outcome after blastocyst transfer: a population-based registry study Presented orally at the 36th Society for Maternal-Fetal Medicine Annual Pregnancy Meeting, Atlanta, GA, Feb. 1–6, 2016. Am J Obstet Gynecol. 2016;214(3):378.e1–378.e10.
Kultursay N, Yalaz M, Koroglu OA. Neonatal outcome following new assisted reproductive technology regulations in Turkey—a nationwide multicenter point prevalence study. J Matern-Fetal Neonatal Med. 2015;28(2):204–9.
Pelkonen S, Hartikainen A, Ritvanen A, Koivunen R, Martikainen H, Gissler M, et al. Major congenital anomalies in children born after frozen embryo transfer: a cohort study 1995–2006. Hum Reprod. 2014;29(7):1552–7.
Pinborg A, Loft A, Henningsen A, Rasmussen S, Andersen A. Infant outcome of 957 singletons born after frozen embryo replacement: the Danish National Cohort Study 1995–2006. FERTILITY AND STERILITY. 2010;94(4):1320–7.
Allen C, Bowdin S, Harrison RF, Sutcliffe AG, Brueton L, Kirby G, et al. Pregnancy and perinatal outcomes after assisted reproduction: a comparative study. Ir J Med Sci. 2008;177(3):233–41.
Westergaard H, Johansen A, Erb K, Andersen A. Danish national in-vitro fertilization registry 1994 and 1995: a controlled study of births, malformations and cytogenetic findings. Hum Reprod. 1999;14(7):1896–902.
Woldringh GH, Horvers M, Janssen AJWM, Reuser JJCM, de Groot SAF, Steiner K, et al. Follow-up of children born after ICSI with epididymal spermatozoa. Hum Reprod. 2011;26(7):1759–67.
Lambalk CB, van Hooff M. Natural versus induced twinning and pregnancy outcome: a Dutch nationwide survey of primiparous dizygotic twin deliveries. Fertil Steril. 2001;75(4):731–6.
Caserta D, Bordi G, Stegagno M, Filippini F, Podagrosi M, Roselli D, et al. Maternal and perinatal outcomes in spontaneous versus assisted conception twin pregnancies. European journal of obstetrics & gynecology and reproductive biology. 2014;174:64–9.
Isaksson R, Gissler M, Tiitinen A. Obstetric outcome among women with unexplained infertility after IVF: a matched case-control study. Hum Reprod. 2002;17(7):1755–61.
Oldereid NB, Hanevik HI, Bakkevig I, Romundstad LB, Magnus Ø, Hazekamp J, et al. Pregnancy outcome according to male diagnosis after ICSI with non-ejaculated sperm compared with ejaculated sperm controls. Reprod Biomed Online. 2014;29(4):417–23.
Hansen M, Kurinczuk JJ, De Klerk N, Burton P, Bower C. Assisted reproductive technology and major birth defects in Western Australia. Obstet Gynecol. 2012;120(4):852–63.
Davies M, Moore V, Willson K, Van Essen P, Priest K, Scott H, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012;366(19):1803–13.
Thalluri V, Woodman R, Vollenhoven B, Tremellen K, Zander-Fox D. Exposure to corticosteroids in the first trimester is associated with an increased risk of urogenital congenital anomalies. Hum Reprod. 2022;37(9):2167–74.
Halliday J, Ukoumunne O, Baker H, Breheny S, Jaques A, Garrett C, et al. Increased risk of blastogenesis birth defects, arising in the first 4 weeks of pregnancy, after assisted reproductive technologies. Hum Reprod. 2010;25(1):59–65.
Davies MJ, Rumbold AR, Marino JL, Willson K, Giles LC, Whitrow MJ, et al. Maternal factors and the risk of birth defects after IVF and ICSI: a whole of population cohort study. BJOG Int J Obstet Gynaecol. 2017;124(10):1537–44.
Hansen M, Kurinczuk JJ, Bower C, Webb S. The risk of major birth defects after intracytoplasmic sperm injection and in vitro fertilization. New Engl J Med. 2002;346(10):725–30.
Basso O, Shapiro GD, Gagnon R, Tamblyn R, Platt RW. Type of infertility and prevalence of congenital malformations. Paediatr Perinat Epidemiol. 2024;38(1):43–53.
Heisey AS, Bell EM, Herdt-Losavio ML, Druschel C. Surveillance of congenital malformations in infants conceived through assisted reproductive technology or other fertility treatments. Birth Defects Research Part A - Clinical and Molecular Teratology. 2015;103(2):119–26.
Luke B, Brown MB, Wantman E, Forestieri NE, Browne ML, Fisher SC, et al. The risk of birth defects with conception by ART. Hum Reprod. 2021;36(1):116–29.
Kelley-Quon L, Tseng C, Janzen C, Shew S. Congenital malformations associated with assisted reproductive technology: A California statewide analysis. J Pediatr Surg. 2013;48(6):1218–24.
Liberman R, Getz K, Heinke D, Luke B, Stern J, Declercq E, et al. Assisted reproductive technology and birth defects: effects of subfertility and multiple births. Birth defects research. 2017;109(14):1144–53.
Wen S, Leader A, White R, Léveillé M, Wilkie V, Zhou J, et al. A comprehensive assessment of outcomes in pregnancies conceived by in vitro fertilization/intracytoplasmic sperm injection. European journal of obstetrics & gynecology and reproductive biology. 2010;150(2):160–5.
Shevell T, Malone F, Vidaver J, Porter T, Luthy D, Comstock C, et al. Assisted reproductive technology and pregnancy outcome. OBSTETRICS AND GYNECOLOGY. 2005;106(5):1039–45.
Chaabane S, Sheehy O, Monnier P, Fraser W, Bissonnette F, Trasler JM, et al. Ovarian stimulation, intrauterine insemination, multiple pregnancy and major congenital malformations: A systematic review and meta- analysis- the ART_rev study. Curr Drug Saf. 2016;11(3):222–61.
Hwang S, Dukhovny D, Gopal D, Cabral H, Missmer S, Diop H, et al. Health of infants after ART-treated, subfertile, and fertile deliveries. Pediatrics. 2018;142(2):e20174069.
Welmerink DB, Voigt LF, Daling JR, Mueller BA. Infertility treatment use in relation to selected adverse birth outcomes. Fertil Steril. 2010;94(7):2580–6.
Palermo GD, Neri QV, Takeuchi T, Squires J, Moy F, Rosenwaks Z. Genetic and epigenetic characteristics of ICSI children. Reprod Biomed Online. 2008;17(6):820–33.
Altal OF, Aleshawi AJ, Khrais MZ, Alkilany BM, Abudalo TM, Al Sharie AH, et al. The practice of intracytoplasmic sperm injection in Jordan: a clinical outcome study. Ann Med Surg. 2020;57:196–200.
Hwang S, Dukhovny D, Gopal D, Cabral H, Diop H, Coddington C, et al. Health outcomes for Massachusetts infants after fresh versus frozen embryo transfer. FERTILITY AND STERILITY. 2019;112(5):900–7.
Shechter-Maor G, Czuzoj-Shulman N, Spence A, Abenhaim H. The effect of assisted reproductive technology on the incidence of birth defects among livebirths. Archives of gynecology and obstetrics. 2018;297(6):1397–403.
Luke B, Gopal D, Cabral H, Stern JE, Diop H. Pregnancy, birth, and infant outcomes by maternal fertility status: the Massachusetts Outcomes Study of Assisted Reproductive Technology. Am J Obstet Gynecol. 2017;217(3):327.e1-327.e14.
Luke B, Stern J, Kotelchuck M, Declercq E, Anderka M, Diop H. Birth outcomes by infertility treatment: analyses of the population-based cohort Massachusetts outcomes study of assisted reproductive technologies (MOSART). J Reprod Med. 2016;61(3):114–27.
Xiong X, Dickey R, Buekens P, Shaffer J, Pridjian G. Use of intracytoplasmic sperm injection and birth outcomes in women conceiving through in vitro fertilization. PAEDIATRIC AND PERINATAL EPIDEMIOLOGY. 2017;31(2):108–15.
Dar S, Librach C, Gunby J, Bissonnette F, Cowan L, Soc CFA. Increased risk of preterm birth in singleton pregnancies after blastocyst versus Day 3 embryo transfer: Canadian ART Register (CARTR) analysis. HUMAN REPRODUCTION. 2013;28(4):924–8.
Shavit T, Oron G, Weon-Young S, Holzer H, Tulandi T. Vitrified-warmed single-embryo transfers may be associated with increased maternal complications compared with fresh single-embryo transfers. Reprod BioMed Online. 2017;35(1):94–102.
Moses X, Torres T, Rasmussen A, George C. Congenital anomalies identified at birth among infants born following assisted reproductive technology in Colorado. BIRTH DEFECTS RESEARCH PART A-CLINICAL AND MOLECULAR TERATOLOGY. 2014;100(2):92–9.
Havelock J, Aaris Henningsen AK, Mannaerts B, Arce JC. ESTHER-1 and ESTHER-2 Trial Groups. Pregnancy and neonatal outcomes in fresh and frozen cycles using blastocysts derived from ovarian stimulation with follitropin delta. J Assist Reprod Genet. 2021;38(10):2651–61.
Sullivan EA, Chughtai AA, Lui K, Wang YA. Morbidity and mortality among very and extreme preterm singletons born following assisted conception in Australia: a population study. Hum Reprod. 2015;30((Sullivan E.A.; Wang Y.A.) University of Technology Sydney, Faculty of Health, Sydney, NSW, Australia):i57.
Henningsen AKA, Spangmose AL, Bay B, Kesmodel U, Pinborg A. Children born after assisted reproduction. Ugeskr Laeger. 2021;183(48):V05210475.
Lu Y, Liu L, Zhang P, Sun Y, Ma C, Li Y. Risk of birth defects in children conceived with assisted reproductive technology: a meta-analysis. Medicine (Baltimore). 2022;101(52):e32405.
W J, J J, D C, D J, L Y, X Y, et al. Birth defects in children conceived by in vitro fertilization and intracytoplasmic sperm injection: a meta-analysis. Fertility and sterility [Internet]. 2012 Jun [cited 2024 Apr 5];97(6). Available from: https://pubmed.ncbi.nlm.nih.gov/22480819/
Assisted reproduction and congenital malformations: a systematic review and meta‐analysis - Veeramani - 2024 - Congenital Anomalies - Wiley Online Library [Internet]. [cited 2024 Jul 23]. Available from: https://onlinelibrary.wiley.com/doi/10.1111/cga.12561.
Salbaum JM, Kappen C. Neural tube defect genes and maternal diabetes during pregnancy. Birth Defects Research Part A, Clinical and molecular teratology. 2010;88(8):601–11.
Field AP. The problems in using fixed-effects models of meta-analysis on real-world data. Underst Stat. 2003;2(2):105–24.
Dettori JR, Norvell DC, Chapman JR. Fixed-effect vs random-effects models for meta-analysis: 3 points to consider. Global Spine J. 2022;12(7):1624–6.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril. 2011;96(2):344–8.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal. No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the work reported. Individual author contributions are as follows: conceptualization: AG; literature screening, data extraction, and data synthesis: PB and AG; statistical analysis: PB and VL; manuscript writing—original draft preparation: PB; manuscript writing—review and editing: AG; intellectual inputs: AG, VSD, VL, SU, SKA, PA, PK; supervision: AG.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhat, P., Dhyani, V.S., Lakshmi, V. et al. Congenital anomalies observed in children conceived through assisted reproductive technology—a systematic review and meta-analysis. J Assist Reprod Genet 42, 1547–1565 (2025). https://doi.org/10.1007/s10815-025-03454-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-025-03454-0